Initial Direct Care Staff Training
Welcome to the online training program that will help you learn the basic skills and information to become a direct care staff person.
This training is required before you can provide unsupervised consumer care. The personal care home and assisted living residences regulations relating to direct care staff person training and orientation require this training.
It is important to read each module carefully because the test at the end will include questions from each of the modules.
The online test at the end of the training has 50 questions. You will need to score 70 percent or above to pass. To score 70 percent, you must get 35 questions correct. You can take the test as many times as you like, and each time you take the test, the questions will be different.
Once you pass the test, you will receive a “certificate of completion” that you must give to your employer.
Let’s get started!
Understanding HIPAA and Confidentiality
(Sources: My Learning Center/ Milestone Home Care Policy)
The individuals in your care are vulnerable in many ways. And it is your responsibility to protect them from injuries, illness, abuse, and violations of their privacy.
What is HIPAA?
HIPAA is the Health Insurance Portability and Accountability Act of 1996. The federal government made very specific rules for protecting private information about any individual in your care. Putting those rules into practice can be challenging, especially when caring for someone in their home. Enabling people to feel comfortable sharing their complete information and health history to provide the best care to them. So, for people to feel comfortable, they need to know that we will protect their information and not share it with people who don’t have a “need to know” about it.
HIPAA defines certain health information as protective. This Protective Health Information or PHI includes things like name, address, social security number, and date of birth. It also includes medical diagnoses, medical history, medications, and any information that could identify the consumers. HIPAA regulations require an employer to appoint a compliance officer to develop and oversee the day-to-day procedures that make compliance possible. And everyone is responsible for making sure that the privacy rules are followed.
The responsibility of protecting the health information of the individual should be a main concern of the agency and its employees, as well as all direct care aides that care for the individual. With so much information being passed among direct care aides and the agency, determining who needs that information and exactly how much they need it becomes critical.
Who should have access to consumers’ protected health information?
Client records must be kept confidential and, except in emergencies, may not be accessible to anyone without the participant’s written consent or if a court orders disclosure other than the following as per § 52.29.
- The participant.
- The participant’s legal guardian.
- The provider staff for the purpose of providing a service to the participant.
- An agent of the Department.
- An individual holding the participant’s power of attorney for health care or health care proxy.
You must be very careful about the role of the person who’s asking you for this information before you disclose anything. Even when someone has the right to know the information about the consumer, it’s still important to share only the information that person “needs to know” without going into further detail. In fact, the term “need to know” is an important concept in HIPAA compliance.
“Need to know” refers to someone having an actual genuine “need to know” certain information to provide adequate care and services. Infection control is a great example of a “need to know” scenario. You need to determine who is at risk for contracting a certain condition, and then, from there, you build your procedures in terms of who needs to know the information and to what level. You don’t necessarily need to say what infections someone has. You just need to say there is an infection control risk or concern, and these are the precautions that you need to take. You do not need to disclose specific symptoms or conditions.
In terms of “need to know,” it’s just enough to be able to provide care and services and protect yourself. But being very careful does not mean that you must get actual diagnoses. A sensitive issue in their past in dealing with family members, whether it be an abusive issue or addiction issue or things like that, we don’t disclose those conditions. We only disclose what the staff would need to know to be able to care for that person. For instance, someone who has, perhaps, had sexual assault in their history and is wary of male caregivers, and then what we disclose is that this person always needs to have a female caregiver. So, we disclose those things but not the reason behind them because you really don’t need to know to be able to provide the care.
Protecting confidential information in the home can be challenging. But good work habits can make it second nature. Here are some important habits to build into your routine.
Important Habits
- Find a private place to discuss the consumer’s care.
- Be aware of how loud you’re talking, even behind closed doors.
- Make sure phone conversations are discreet and to the point.
- When using a printer, retrieve information immediately and use it, store it, or dispose of it.
- Store medical records in a secured area.
- Conceal all medical records even as they are being used.
Consumer Control and Independent Living Philosophy
The independent living philosophy holds that individuals have the right to live with dignity and appropriate support in their homes. They choose to control and make decisions about their lives by fully participating in their communities. One of the keys to a successful relationship between a direct care worker and a consumer is helping the consumer live as independently as possible.
The independent living philosophy is based on the followings:
- Consumer’s choice
- Communication
- Independence
- Dignity of Risk
Communication is paramount in any successful relationship because it helps establish that independence. When a consumer goes to a nursing home, she will lose that independence. They have to abide by the policies of the nursing home. For example, if 8 o’clock is the time for breakfast, you have got to get out of bed, sit in your wheelchair, and go for breakfast, which is not the case at home. At home, you will experience true independence. You are not going to get it when you are institutionalized.
DCW is encouraged to give the consumers as much independence as is safe. So, when do you want your lunch? When do you want a bath? They are making those decisions. They have the right not to have lunch. And that’s their choice, which we cannot enforce upon them. As human beings, if somebody tells us what to do every minute of the day, that’s not independence. At times, getting the consumer to eat can be difficult. However, coercing consumers to do things they are not ready for is against the choice of the consumers. They have every right to choose what is appropriate for them. DCW cannot act as the boss.
Inappropriate approach to handle a situation:
DCW: “All right, it’s time for you to eat lunch.”
Consumer, “No, I am fine now.”
DCW: “You have to.” “I have already put it on your table.”
Appropriate handling of the same situation:
DCW, “Okay, Mrs. Smith, are you ready for lunch?”
Consumer, “No, no, no.” “I am not hungry now.”
DCW: “May I serve you later, then?”
Consumer, “Maybe you could do that, or I will let you know, okay?”
If a consumer can respond and is not cognitively impaired, then the DCW is only responsible to the consumer. If the consumer has communication issues or has a cognitive disability, then the DCW may be required to be directed by a family member. Situations with relatives or other caregivers must be handled appropriately.
Here is an example of inappropriate dealing:
Family: “Hey, I told you she should be given lunch at 12:30 pm.”
DCW: “She doesn’t want to eat it.”
Family: “I specifically gave you the direction that she should be eating around that time.”
DCW: “Wait, what am I supposed to do if she does not want to eat, then?” Should I force myself on her?
Here is the more appropriate way to handle a situation:
Family: “Hey, I suppose she should eat by 12:30?”
DCW: “I respect her choice, as she wanted to eat a little later because she says her stomach is still full.” You can talk to her if you want to.”
Family: “Okay, that makes sense.” “I’m fine with it if she wants to.”
The relationship with the consumer we work with needs to be a partnership. Our goal should be to make consumers feel safe and comfortable at home. DCW is always encouraged to be flexible or adaptable to the needs and desires of the consumers as long as it is safe for them. DCW must partake in the consumers’ plan of care.
Sometimes, the consumer may prefer not to stay out of bed and go to the table for breakfast. Instead, they may like to eat sitting in bed.
Inappropriate approach:
DCW: “Let’s get out of bed for breakfast.”
Consumer: “No, I am not getting out of bed.”
DCW: “You must because I am tired of bringing food daily.” “You may also have to use the bath.”
Consumer: “No, I am okay here.” “I am going to use the bath later.”
Here is the more appropriate approach:
DCW: “Mrs. Smith, are you ready to get out of bed?”
Consumer: “No, I am fine here.” “I want to stay a little longer here today.”
DCW: “Can I bring breakfast here then?” Or is there anything I can bring before breakfast?”
Consumer: “Not now. Thanks!”
DCW: “Okay then. I am going to do the dishes. If you need anything, give me a call.
Consumer: “Okay. I will let you know.”
DCW: “Okay!”
Although our goal is to allow consumers to enjoy as much independence as possible, sometimes it takes work for DCW to balance consumers’ safety with their right to be independent. DCW needs to talk to the consumers with disabilities and understand their comfort level when we are transferring. Sometimes, consumers’ decisions will have opposite consequences. We need to explain their decisions if they relate to safety and explain the cost of taking risks. Explain that they may fall if they choose to take the risk. However, we should avoid being too hands-on with consumers with disabilities because this may irritate them, and we should prioritize consumer safety. It is always critical to communicate potential risks to customers.
Instrumental activities of Daily Living (IADLs)
Activities of Daily Living (ADLs)
Why is helping consumers with everyday activities so important?
Think about your own daily activities. You perform a series of little tasks each morning routinely as you wake up, such as taking care of your personal hygiene, which includes bathing, showering, grooming, toileting, oral care, etc. Then the next things you do include dressing, undressing, eating, drinking, etc. As the day progresses, you are required to do a series of other activities that involve transferring or mobility. Assume you cannot perform these activities independently due to cognitive or physical limitations. Life becomes tough for you, and you might feel frustrated, helpless, or vulnerable because of a loss in your ability to do these basic things, and you might feel bad about yourself and get angry. In this situation, you will need someone to help you with your activities of daily living (ADLs). For instance, someone needs to help with eating, bathing, grooming, nail care, etc.; help you on your way to and from the toilet; clean; get dressed and undressed; roll onto the side of the bed; swing your legs over the edge of the bed; place your feet on the floor and stand; etc.
As a direct care worker, you can be confident that your service to such consumers will help them ease their ADLs and maintain the quality of their lives if you honor their needs and perform your duties accordingly.
Which activities are important?
Generally, the kinds of activities that are important to a consumer are organized into two groups:
- ADLs (Activities of Daily Living): These are the most basic activities necessary for daily life. They include the following:
- Eating & drinking.
- Ambulating – the ability to move about, such as walking with or without devices like canes, crutches, walkers, etc.
- Transferring – the ability to get in and out of bed, a chair or on and off a toilet.
- Taking medications.
- Personal hygiene – bathing or showering, shampooing hair, brushing teeth.
- Bladder & bowel management.
- Positioning and changing positions in a chair or bed.
- Securing health care.
- IADLs (InstrumentalActivities of Daily Living): These activities are more complex and include:
- Using the telephone.
- Shopping.
- Doing laundry.
- Obtaining and keeping clean clothing appropriate for the season.
- Making and keeping appointments.
- Writing letters or other correspondence.
- Taking part in social and leisure activities.
- Using a prosthetic device – a substitute for a missing body part such as a hand or leg.
- Managing finances.
- Driving or arranging transportation.
As you can see, many activities are part of everyday life. For some of the people you serve, your help with ADLs and IADLs will have a significant impact on their ability to participate in and enjoy life. For others, you will be the only way they are able to complete much of what they need to keep safe and healthy from day to day.
What causes changes in ADLs and IADLs?
Many things can cause a change in a consumer’s ability to perform these basic activities. You will learn more about this in later modules. For right now, it is important to know four basic things about changes in ADLs and IADLs:
- Some consumers have been unable to perform some activities for quite some time—maybe years. These consumers have had a longer time to adjust to their loss. Many also know a great deal about how they like to be helped and have strong preferences. For example, Mr. Smith may like to brush his teeth before combing his hair, or he may like to get dressed by putting on clothes in a particular order, or eat, wake up, or go to bed at a certain time. Wherever possible, it is important to honor these preferences.
- Other consumers have experienced a recent loss of ability. This means that they have had less time to adjust to their losses and may still be learning about how they can best receive help. In some cases, the consumer is also trying to adjust to the fact that they may never recover the abilities they’ve lost. Some consumers have a high ability to adjust to their loss. Others find it more difficult and may display sadness, anger, or frustration. In these cases, it is important to know that the angry things a consumer may say are probably not directed at you but are really anger at the loss. To overcome and adjust to the loss of ability, it is often helpful that consumers have a strong sense that they can still have some control in their everyday lives. For this reason, it is important to involve consumers in choosing how activities will be completed. It is important to encourage them to do as much as they can on their own.
- It is likely that some consumers will have experienced brain damage and will be unable to remember, solve problems, or even be fully aware of what is going on around them. For some of these individuals, each time you interact with them is like the first time. So, your patience and understanding are critical elements of being a caring worker. You must accept and honor that their experiences are real for them. You can also provide hints and suggestions for these consumers. For example, Mr. John forgets to bring a jacket when going outside in cold weather. You can give him a cue by saying, “Mr. John, the weatherman says it is cold outside today.” I’m going to get my jacket. “Would you like me to get yours?”
- A short-term loss of mental or physical capacities will also be experienced by some consumers, from which they will eventually recover. This loss could be from a mental condition, an accident, or the healing process after a procedure. These consumers won’t feel as though they must change their ways of doing things permanently. Thus, their impatience with the healing process is not unusual. Again, when dealing with these folks, you should exercise patience and understanding on your end. They could also require encouragement to put up their best effort as they work toward recovery. To determine how you can best help, you should always review their care plan.
Four general helping rules:
- The care plan is the starting place for knowing what kind of help is needed by each consumer.
Each care plan should give a clear picture of the consumer’s needs and preferences. Always make sure you read and understand the care plan for each consumer you serve. - When you are unsure about preferences or if help is needed, ask.
Sometimes you will observe a consumer struggling with a task, or even after having read the care plan, you may not be sure of the consumer’s needs or preferences. While your immediate impulse might be to simply start helping, it is better to ask first. If you have a consumer who cannot understand or respond to your questions, try to find out from family members or others who know about the consumer’s preferences, and ask your supervisor to record this information in the care plan so it is available to all staff. - Try to use a “person-centered” approach. A “person-centered” approach involves respecting and honoring the uniqueness of each person and respecting that person’s right to be involved in all decisions that impact his or her life. These include minor decisions about how ADLs and IADLs are carried out with your assistance.
- If you believe the consumer is in immediate danger of injury, move to help right away. For example, if a consumer has fallen asleep and is about to fall out of a chair, move to help reposition him or her immediately.
Assistance with mealtime:
Many of the tasks with which you will help consumers have been studied and analyzed to find safe, respectful, and effective ways for you to assist the consumer. In this chapter, you will be introduced to ways to assist someone with eating. Mealtime assistance can be divided into sections. Each is presented below along with the steps to accomplish it.
1.Preparing the consumer for meal
To help prepare consumers for meals. Here are some ways in which you can help:
- Ask the consumer if he/she would like assistance in brushing his/her hair or putting on make-up.
- Ask the consumer if he/she needs to use the bathroom. Assist the consumer according to his/her needs.
- Assist the consumer in washing his/her hands or face if assistance is needed.
- Ensure that the consumer has his/her dentures on if they wear them.
- Ask the consumer where he/she would like to sit in the dining room.
2. Serving meals and aiding during meals.
While serving meals, keep in mind that your calm, relaxed, friendly, encouraging, and helpful behavior will go a long way toward making mealtime special. Here are the kinds of tasks you may perform:
- Serve the meal to the consumer by calmly and quietly placing it within easy reach.
- Make sure the consumer has all the utensils he/she will need.
- Check the consumer frequently to see if he/she needs help.
- Offer to cut food for a consumer who is having difficulty. When cutting food, always make sure the pieces are small to help prevent choking. A consumer with arthritis may also need help with things such as opening milk containers.
- Offer different food if a consumer refuses what was offered. Each consumer has a right to food that is appealing and nutritionally sound.
- Allow the consumer time to complete one course before starting another.
If you see any of the following, tell your supervisor:
- A change in the amount of assistance a consumer need while eating.
- A change in general behaviors during mealtime such as playing with food, throwing food, or falling asleep.
- A change in attitude such as withdrawing, showing anger or frustration.
- Choking while eating or drinking.
- Eating less or more food than usual.
- A refusal to eat.
If needed, help the consumer check their personal appearance before moving away from the table. For example, check to see if there are any food spills or crumbs that need to be cleaned. Help a consumer to wipe his/her face, if necessary.
In addition to the basic steps already listed, several other things should be considered. First, it is important that the consumers’ cultural preferences and beliefs be considered. For example, you may have a consumer who wants to pray before each meal. While you do not have to pray with the consumer, it is important that you sit quietly and respectfully while the consumer does this. You should also be sensitive to the fact that many people’s food preferences are strongly influenced by their culture, ethnic background, and religion. These preferences should be honored when possible.
Recognizing changes in the consumer that need to be addressed.
(Source: DMCA / Copyright Policy (slidetodoc.com))
Cognitive Impairment
A temporary or permanent change within the brain that affects a person’s ability to think, reason, and learn.
- Temporary causes may include stress, medication, depression, vitamin deficiency, thyroid disease, alcohol, and head trauma.
- Permanent causes include severe head trauma, illness, brain disease, and brain damage at birth.
Disorders that Cause Cognitive Impairment:
Depression– emotional sadness and withdrawal
Anxiety– persistent feelings of fear and nervousness
Suspiciousness– distrust of others
Delusion- a false belief not supported by reality.
Paranoia– irrational feeling of being persecuted, suspiciousness, and hostility.
Schizophrenia– suspiciousness, paranoia, and delusion resulting in inappropriate behavior.
Mental retardation– a process which slows or stops a child’s brain from maturing.
Dementia- progressive mental deterioration due to organic brain disease which causes structural changes within the brain (ex. Alzheimer’s)
Reducing Effects of Advanced Dementia:
Reality Orientation
Helps consumers remain aware of their environment, of time, and of themselves.
Validation Therapy
Helps consumers improve their dignity and self-worth by having their feelings and memories acknowledged.
Reminiscing
Allows consumers to talk about past experiences, especially pleasant ones.
Responses to Difficult Behavior:
Difficult behavior may result from too much stimulation, change in routine or environment, physical pain or discomfort, medication reactions, and fatigue.
1) Remain calm, speak slowly and clearly
2) Avoid approaching the consumer from the side or back
3) Try to calm the consumer by holding hands, patting, and singing (if appropriate)
4) Try to distract the consumer’s attention and redirect behavior
5) Allow the consumer to express feelings (if talking reduces agitation)
Dementia Clients Need Assistance with:
Safety: Monitor the movement, watch for appropriate use of objects, and check that clothing is worn properly
Nutrition: Assist client to dining area when food is served, have food ready, allow consumer extra time to chew and swallow, serve only one food at a time, monitor food intake.
Hydration: Offer fluids more often and in smaller amounts, listen for spoken cues that consumer may be thirsty, watch for nonverbal signs (dry mouth, smacking lips).
Dressing: Choosing appropriate clothing, offer choice of two outfits, assist to dress properly, and simplify dressing according to needs.
Bathing: Prepare the bathing area before bringing a consumer into the room, explain the procedure, check the temperature, and assist the consumer in bathing.
Elimination: Take consumer to bathroom frequently, provide perineal care as needed
Basic Infection Control
As a direct care worker, it is an essential part of your job you remain protected and protect the consumers from infectious diseases. You can only protect the consumers if you protect yourself first. Some consumers have weakened immune systems and are more vulnerable to infectious diseases.
So, what are infectious diseases?
Infectious diseases are disorders caused by organisms such as bacteria, viruses, fungi, or parasites. Many organisms live in the human body. They usually are harmless or helpful. But under certain conditions, some organisms cause diseases. Infectious diseases can pass from person to person through contact, watery fluids, or air. Insects and animals transmit some infectious diseases. Others may be caused by eating contaminated food or water or being exposed to environmental organisms. The infection can be mild, which may only require rest and home remedies, to life-threatening and may need medical attention., including hospitalizations.
DCW’s role is critical in helping to identify early infectious diseases to help communicate infection control techniques to the consumers, their primary caregivers, and communicate to their supervisors.
The signs and symptoms vary depending on the organism causing the infection. However, fever and fatigue are often some of the common symptoms.
Respiratory is common among consumers. There are flu-like symptoms that you need to watch for. They are called flu-like symptoms because they are common in many infectious diseases, some are serious, and others are less serious. The elevated temperature, usually above 100.4 F (38 C), fever, chills and sweats, headache, fatigue, dry and persistent cough, shortness of breath, chest discomfort, myalgia (muscle pain) when you have the flue, sore throat, rhinorrhea (runny nose), nausea, vomiting, and abdominal pain. The appearance any of these symptoms should raise your suspicion about the possible presence of infectious disease. However, this does not guarantee that a consumer has the flu. The most common flu symptoms are fever, chills, coughs, sore throats, muscle aches, and headaches. Consumers will usually complain of fatigue and loss of energy.
Every year we face seasonal or common flu. This is a respiratory illness that can be transmitted from person to person. Most people have some level of immunity. Vaccines are available to prevent this seasonal flu. Practicing infection control with the consumers will avoid spreading the seasonal flu that could be fatal to consumers. Infection is sometimes deadly to consumers, their family members, and caregivers. That’s why understanding infection control is so important. They can be spread through direct contact, coughing or sneezing, talking, body fluids, any drainage from the wounds, etc. Both consumers and direct care workers are at high risk for contracting and transmitting infectious diseases. Since infectious can be very serious for consumers, direct care workers must take steps to ensure that the cause of infection does not spread.
How can you distinguish between a common cold and other severe infectious illnesses?
People with the common cold have low energy and may want to rest. But when they have the flu, they feel very sick and fatigued, with severe headaches and muscle aches. It is also essential to know that extremely frail people may have flu-like symptoms and only a very mild elevation in their temperature. Do not assume that the absence of high fever means they are not severely ill. Their bodies may be too weak to generate fever.
Infectious diseases of the skin and urinary tract can also be very serious.
How can you tell a wound is infected?

Symptoms:
- A fever
- A foul odor near the cut or wound.
- Blood or yellow pus coming from the wound.
- Pain in the affected area
- Warm, red, and swollen skin near the area
Signs and Symptoms of Serious Urinary Tract Infection (UTI)
- UTI is an infection in any part of the urinary system (Kidneys, ureters, bladder, and urethra). Most infection occurs in the lower urinary tract- (bladder and urethra). Women are at greater risk of developing UTI than men.
- Hematuria (blood in urine)
- Urine that looks cloudy
- Elevated temperature (fever)
- Painful urination
- A strong urge to urinate that doesn’t go away.
- Strong-smelling urine
Tuberculosis (TB): Tuberculosis is a potentially serious infectious disease mainly affecting the lungs. It is caused by bacteria (Mycobacterium tuberculosis). Although TB is a highly contagious disease, it is curable and preventable. If not treated properly, TB can be fatal. You must watch for signs of tuberculosis in consumers and your potential exposure. Consumers who are weakened by other illnesses are more vulnerable and prone to getting infected. Consumers with aids/HIV and certain cancers are prime candidates to develop active TB. Symptoms of TB depend on where the TB bacterium is growing in the body. The symptoms of TB:
- Fever
- Chills
- Chest pain
- Weight loss
- Night sweats
- Breathlessness
- Loss of appetite
- Excessive fatigue
- Coughing up mucous streaked with blood
- A persistent cough that lasts three weeks or longer
Intestinal Infections: Infections of the intestinal tract can also be highly contagious. One of the common infections contracted by hospitalized consumers is Clostridioides difficile (Clostridium difficile), more commonly called C. diff. The risk is greater for people who:
- Are taking a large course of antibiotics or have recently taken them.
- Have spent time in a hospital or long-term care facility (nursing home)
- Have a weakened immune system.
- Are 65 years of age or older.
Mild Infection
- Watery diarrhea 3 or more times a day for more than 1 day
- Mild abdominal cramping and tenderness
Moderate to Severe Infection
- Watery diarrhea, as often as 10 to 15 times a day
- Abdominal cramping and pain, which may be severe
- Rapid heart rate
- Dehydration
- Fever
- Nausea
- Increased white blood cell count
- Kidney failure
- Blood or pus in the stool
How do you get C. diff?
- By direct contact with someone who has the germs
- By indirect contact. If you come into contact with a caregiver of someone with C. diff, they may have picked up the germs and could pass them on
- By touching contaminated surfaces that have germs on them
Skin Infections: Not all skin infections are infectious. However, if you notice a new rash in consumers, you must report it to the agency. Bedsores or pressure ulcers are common sights of infection. Pressure ulcers are injuries to the skin and underlying tissue resulting from prolonged pressure on the skin. People at risk of bedsores have medical conditions that limit their ability to change positions. Most bedsores heal with treatment. Some never heal completely. If not prevented, the infection can spread to the rest of the body, causing fever, chills, and confusion.
Warning Symptoms of Pressure Ulcers:
- Unusual changes in skin color or texture
- Swelling
- Pus-like drainage with a foul smell
- An area of skin that feels cooler or warmer to the touch than other areas
- Tender areas
Common Sites of pressure ulcers:
- Tailbone or buttocks
- Shoulder blades and spine
- Backs of arms and legs where they rest against the chair
In Bed:
- The back or sides of the head
- The shoulder blades
- The hip, lower back, or tailbone
- The heels, ankles, and skin behind the knees.
The best way to prevent pressure ulcers is to ensure the consumer does not get pressure ulcers at all.
Scabies
Scabies is another skin disease and can quickly spread through close person-to-person contact. Scabies is an itchy skin rash caused by a tiny burrowing mite called Sarcoptes scabiei. Although scabies is not life-threatening to a healthy person, it can be severe to those whose immune is compromised.
Signs and Symptoms of scabies:
- Itching, often severe and usually worse at night
- Thin, wavy tunnels made up of tiny blisters or bumps on the skin.
Where is scabies found?
- Between the fingers and toes
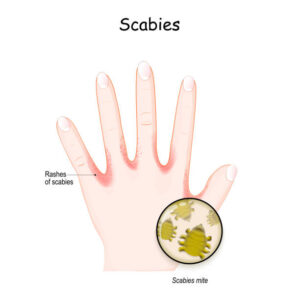
Scabies mite. Human’s hand. skin with Rashes. seven-year itch is a contagious skin infestation by the mite Sarcoptes scabiei. Close-up of Scabies mite. Vector illustration - In the armpits
- Around the waist
- Along the insides of the wrists
- On the inner elbows
- On the soles of the feet
- On the chest
- Around the nipples
- Around the belly button
- Around the genitals
- In the groin area
- On the buttocks
Chickenpox: Chickenpox is an infection caused by the varicella-zoster virus. It causes an itchy rash with small, fluid-filled blisters. It is highly contagious to consumers who haven’t had the disease or been vaccinated against it. There are vaccines available to prevent getting chickenpox.
This disease progresses through symptoms that start one to three weeks after exposure to the virus, including:
- Flu-like symptoms include fever, fatigue, loss of appetite, body aches, and headache. These symptoms typically start a day or two before a rash appears.
- Red spots appear on the face and chest, eventually spreading over the entire body. The red spots develop into itchy, fluid-filled blisters.
- Blisters weep, become sores, form crusts, and heal. As some of the blisters form crusts.
Some basic ways to control infectious diseases:
Good hand hygiene is essential:
The first step to prevent the spread of infectious disease is to practice good hand-washing hygiene. Another thing direct care workers can do to reduce the spread of germs is to limit their wearing of jewelry. This is because the tiny surfaces and crevices on rings and other jewelry can serve as a breeding ground for germs. If you choose to wear a ring, keep it simple. Since fingernails can serve as a breeding ground for germs, keep your nails short and clean.
When to wash hands:
- Before and after wearing gloves.
- At the start of the workday and several times throughout the day.
- When your hands are visibly soiled (dirty) or contaminated with blood or body fluids.
- Before having direct contact with the consumer’s skin.
- After having direct contact with the consumer’s skin, especially when the skin has wounds or is broken.
- After assisting with toileting or changing incontinence products from the consumer.
- After the direct care worker uses the restroom.
- Before eating.
- Before preparing food.
- Before serving food.
- After wiping the nose, sneezing, or touching the face.
- After smoking.
How to wash hands properly:
- Wet your hands under warm, running water.
- Rub your hands with soap and work up a good lather to all surfaces from 2 inches above the wrists for at least 20 seconds.
- Wash the palms, sides, and back of your hands, between your fingers, thumbs, and under your fingernails.
- Rub the nails of each hand across the palm to remove dirt from under the fingernails.
Repeat steps 3 and 4 for 20 seconds.
- Rinse your hands under warm running water. Make sure you get all the soap off.
- Dry your hands with a clean towel or paper towel. Pat your hands, and work back toward your forearms.
- Turn the faucet off with the paper towel and use the paper towel to open the door as you leave the restroom so that you do not pick up germs that may exist on the handle.
Using gloves to reduce the risk of infection:
As a direct care staff, you should use gloves when there is the possibility that you will have contact with blood, other potentially infectious material, or items, and surfaces contaminated with these materials. Wear gloves to carry soiled or contaminated materials and carry the material so it does not touch any other surface, including your clothing. It is important to dispose of soiled material as soon as possible. For example, put soiled linens directly into the designated container and not on the floor.
Putting on and taking off gloves:
Before putting gloves on, remove all sharp jewelry and wash your hands to remove germs. When putting the gloves on, begin by putting your fingers into the tips and then pulling the entire glove over your clean hand. Remove gloves by pulling the glove inside out so that whatever has touched the glove remains untouched by your exposed skin.
Cleaning and disinfecting – Keeping germs away:
Another critical method for preventing the spread of germs is cleaning and disinfecting surfaces. Cleaning refers to washing with soap and water, and disinfecting refers to using a cleaning product that kills bacteria and other germs. Disinfection is especially important in the kitchen and bathroom.
Some general steps are involved in the proper cleaning and disinfection of surfaces:
- Carefully follow directions and precautions on all cleaning products.
- Begin cleaning the surface thoroughly with soap and water or another cleaner.
- After cleaning, if you need to use a disinfectant, apply it to the area and let it stand for a few minutes or longer, following the directions on the product.
- Wipe the surface with a paper towel that can be thrown away or a cloth that will be washed immediately afterward.
- After cleaning or disinfecting, always wash your hands, even if wore gloves.
Universal Precautions
Universal precautions is an approach to infection control to treat all human blood and certain human body fluids as if they were known to be infectious for HIV, HBV, and other bloodborne pathogens, (Bloodborne Pathogens Standard 29 CFR 1910.1030(b) definitions).
The general rule to universal precaution is that ALL staff should follow Universal Precautions at ALL times on ALL persons. Universal Precautions should be used for handling or cleaning-up blood and other potentially infectious material, such as soiled diapers, bandages, etc. When universal precautions are followed correctly, they can significantly decrease the likelihood that a healthcare worker will contract a disease from a consumer they are working with.
Employee exposure to bloodborne pathogens from blood and Other Potentially Infectious Materials (OPIM) because employees are not using Universal Precautions.
- Bloodborne pathogens are pathogenic microorganisms that are present in human blood and can cause disease in humans.
- Some infections that can be transmitted through contact with blood and body fluids include:
- HIV, Hepatitis A, B, C, Staph and Strep infections, Gastroenteritis-salmonella, and shigella, Pneumonia, Syphilis, TB, Malaria, Measles, Chicken Pox, Herpes, Urinary tract infections, and Blood infections. The greatest risks are from HIV and Hepatitis B and C.
Possible Solutions
Use Universal Precautions. (Source: Toolbox talk week of 10/9/2017-Universal Precautions- Bloodborne Pathogens | ToolBox-Talk (wordpress.com)
Bloodborne Pathogen Standard 29 CFR 1910.1030(d)(1) requires:
- Employees to observe Universal Precautions to prevent contact with blood or other potentially infectious materials (OPIM).
- Under circumstances in which differentiation between body fluid types is difficult or impossible, all body fluids shall be considered potentially infectious materials.
- Treat all blood and other potentially infectious materials with appropriate precautions such as:
- Use gloves, masks, and gowns if blood or OPIM exposure is anticipated.
- Use engineering and work practice controls to limit exposure.
OPIM is defined in 29 CFR 1910.1030(b) as:
- The following human body fluids: semen, vaginal secretions, cerebrospinal fluid (the fluid that surrounds the brain and spinal cord), synovial fluid (the fluid found in the joints), pleural fluid (the fluid that surrounds the lungs), pericardial fluid (the fluid that surrounds the heart), peritoneal fluid( the fluid found in the abdominal cavity), amniotic fluid ( the fluid that surrounds a fetus as it develops in the uterus), saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids;
- Any unfixed tissue or organ (other than intact skin) from a human (living or dead); and
- HIV-containing cell or tissue cultures, organ cultures; HIV- or HBV-containing culture medium or other solutions; and blood, organs, or other tissues from experimental animals infected with HIV or HBV.
The Bloodborne Pathogens Standard allows for hospitals to use acceptable alternatives [OSHA Directive CPL 02-02-069, (2001, November 27)] to universal precautions:
- Alternative concepts in infection control are called Body Substance Isolation (BSI) and Standard Precautions. These methods define all body fluids and substances as infectious. These methods incorporate not only the fluids and materials covered by the Bloodborne Pathogens Standard but expand coverage to include all body fluids and substances.
- These concepts are acceptable alternatives to universal precautions, provided that facilities utilizing them adhere to all other standard provisions.
- For compliance with OSHA Standards, the use of either Universal Precautions or Standard Precautions is acceptable.
The CDC recommends Standard Precautions for the care of all consumers, regardless of their diagnosis or presumed infection status.
- Standard Precautionsapply to 1) blood; 2) all body fluids, secretions, and excretions, except sweat, regardless of whether they contain visible blood; 3) non-intact skin; and 4) mucous membranes. Standard precautions are designed to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources of infection in hospitals.
- Standard precautions include the use of: hand washing and appropriate personal protective equipment such as gloves, gowns, and masks whenever touching or exposure to consumers’ body fluids is anticipated.
- Transmission-Based Precautions (i.e., Airborne Precautions, Droplet Precautions, and Contact Precautions) are recommended to provide additional precautions beyond Standard Precautions to interrupt the transmission of pathogens in hospitals.
- Transmission-based precautions can be used for consumers with known or suspected to be infected or colonized with epidemiologically important pathogens that can be transmitted by airborne or droplet transmission or by contact with dry skin or contaminated surfaces. These precautions should be used in addition to standard precautions.
- Airborne Precautions used for infections spread in small particles in the air, such as chicken pox.
- Droplet Precautions are used for infections spread in large droplets by coughing, talking, or sneezing, such as influenza.
- Contact Precautions used for infections spread by skin-to-skin contact or contact with other surfaces such as herpes simplex virus.
- Transmission-based precautions can be used for consumers with known or suspected to be infected or colonized with epidemiologically important pathogens that can be transmitted by airborne or droplet transmission or by contact with dry skin or contaminated surfaces. These precautions should be used in addition to standard precautions.
- Airborne Precautions, Droplet Precautions, and Contact Precautions. May be combined for diseases that have multiple routes of transmission. When used either singularly or in combination, they are to be used in addition to Standard Precautions.
Handling of Emergencies
Working in consumers’ homes sometimes is unpredictable. So as a caregiver, you must be watchful of your surroundings as you never know anything could happen at any time. If you are in such situation (s), you must handle the situation with an emergency (quick action). An emergency demands you to act quickly and appropriately that is right for that situation. Things that you should consider while handling an emergency are:
- Notice or Record what, where, and when. This does not take more than a few seconds but is crucial. You may end up doing the wrong thing without thinking. However, if you cannot do anything, call 911, and report to them what happened and when. They will take care of the rest.
- As a direct care worker, it is important to recognize warning emergencies in consumers, such as heart attack or stroke. Your reaction and ability to handle the situation will make a difference in the life or death of consumers. If you observe the following warning signs of a heart attack or a stroke, you must call 911 and notify the incident to your supervisor. You could ensure they are not hurting themselves and remain vigilant until 911 arrives. Give the operator the telephone number, street address, and directions to the consumer’s home. You should write this information in advance and post it near the telephone or on refrigerators in the house where it is visible or easily accessible.
- If a consumer is not acting normally, it is advisable to talk to the consumer and, if needed, advise them to get evaluated by visiting the emergency room (ER). Sometimes, timely intervention or action can save the consumer’s life.
- It is critical to assess the situation every time you enter the consumer’s home. You can ask the consumer how they are doing or feeling to understand their situation and what you might need to do. If you observe any of the following signs in the consumers, and if you feel any life-threatening or eminent emergency, the best thing you can do is call 911.
Warning Signs of a Heart Attack
Warning Signs of a Stroke:
- Sudden numbness
- Weakness of the face, arm, or leg
- Confusion or trouble speaking
- Blurred vision
- Trouble walking
- Dizziness
- Severe headache
Falling: One of the most significant emergencies in a consumer’s home is falling. You can do many things to prevent the consumer from falling.
You can do the following:
- Ensure rugs and carpets are secured

- Check for clutter
- Make sure there is enough lighting
- Make sure chairs and couches are easy to get out of
- Check for electrical cords or telephone cords getting on the way
As snow and icy road roads can be another risk for falling. We should ask consumers to wear proper footwear to prevent slipping and falling.
What can you do when they fall:
- Try to communicate with the consumer.
- If they can move, you can assist them to move.
- If they cannot move, do not insist on them moving. You can call 911 in this case.
Oxygen and Smoking
One of the changing things in the case of some consumers is smoking and using oxygen. This is a hazardous situation. Someone can blow up if allowed to do so. Any heat source (cooking/ heating) could be an issue when a consumer uses oxygen. Your safety and consumer’s safety will be at risk.
If your consumer refuses to stop smoking while on oxygen, do not unplug their oxygen. Call your supervisor immediately for further instructions. You may be instructed to leave the house immediately.
If there is a small fire and you have access to a fire extinguisher, you can extinguish the fire. But anything beyond this, it is vital for you and the consumer to get out of the home safely and call 911 immediately. It is also essential to conduct regular fire drills with your consumer. Check the fire alarm, if installed, and check the smoke detector regularly. If you smell any odors that seem very suspicious or dangerous, call 911 immediately and get yourself and your consumer out of the home.
Safety risk in the consumer’s home:
Your safety is as important as the safety of the consumers. As a home care aide, you face numerous hazardous situations. You must be watchful and remain informed about the surroundings at all times. Falling in or out of the home and overexertion are the most common challenges home care aides face. When you’re lifting, we should know how to lift. It is important always to tell the consumer what you are going to do before you do it. Sometimes, people with the cognitively impaired do not know what they are going to do and when they are going to do it. Their senses may be a lot different than ours.
The following are some major safety concerns for caregivers.
- Falls
- Overexertion (Improper or repetitive lifting and repositioning, given the nature of the task, sometimes cause overexertion to the caregivers)
- Unsafe surroundings
- Hostile Pets
- Guns
- Inclement weather
Unsafe Surroundings:
If you feel unsafe at the consumer’s home, in the surroundings, or imminent danger, you must take quick and proper action to ensure your safety. You should assess the situation if the consumer lives in an unsafe neighborhood. If you feel unsafe, you should not enter the house. Instead, call your supervisor immediately for further instructions. If you are in a situation where there is domestic violence or physical abuse, you must leave and contact your supervisor immediately.
Animals:
Animals can be very harmful to home care workers. Animals should be locked up; if they are not and your consumer refuses to do so, call your supervisor immediately for further instructions. Never touch any animals, no matter how small or cute they are. They could carry diseases.
Guns
Consumers have the right to keep guns legally. However, the guns should be locked up and completely out of sight for safety reasons. If the consumer refuses to comply, call your supervisor immediately for instructions.
Bad Weather
Bad weather can be an issue for home caregivers. You must use good judgment and try your best to get to your consumer’s home, but you cannot compromise your safety. You are advised to get emergency kits or supplies (water, blankets, etc.) for protection in case you are stranded in bad weather.
(Source: My Learning Center)
Documentation
Documentation, or rather ‘good’ client documentation, is the cornerstone of quality care outcomes. Well written care plans along with detailed progress or case notes both support and demonstrate quality care. Good client documentation is essential for numerous reasons, including giving your clients the best possible care.
So, what are the main reasons for documenting?
Communication:
Client documentation is an effective method of sharing information amongst staff and other service providers. In the world of Consumer Directed Care there may be more than one service provider supporting an individual, so it’s best for everyone to be on the same page.
Assessment:
Coordinators and case managers can use client progress notes as a primary reference source when conducting a re-assessment. They can utilize the information to measure how well a particular approach is meeting the individual’s stated goals. Notes may also indicate improvement or deterioration of the individual and prompt changes in service delivery or identify needed referrals.
Continuity of Care:
As well as being useful for effective communication, good documentation helps all staff to understand the current care needs of a client. This in turn promotes continuity of support and care. Documentation can be used to prompt or remind staff or family members of specific actions. For example, when regular staff go on holidays and a relief support worker is brought in.
Shared Knowledge:
Think about a time when you have either been in hospital or visited a family or friend in hospital. Staff, including doctors, work different shifts and a consumer may be seen and supported by a number of different staff members during the period of their stay. Client documentation allows each staff member to understand the medical history of the individual and any interventions that are relevant to their care and support needs. This history can then be used to direct future interventions and actions. Organizations that provide aged care services also rely on this ability to share relevant information between staff to promote quality outcomes.
Continuous Quality Improvement:
This is an important aspect of providing quality care. Although there are identified standards that support the industry, you’re your organization might be currently assessed as meeting these, you cannot become complacent. The expectations of individuals and their families’ change. Good documentation can assist in picking up trends in the needs of an individual, your target consumer group and the needs of your workforce going forward.
Physical Evidence:
‘If it isn’t written down, it never happened.’
Without documentation, you have no concrete evidence of services delivered or interventions implemented. Some organizations fail their quality audit/review, primarily because they cannot prove they delivered services due to poor client documentation.
So,
- while you can provide the best possible care and support to an individual,
- while you might meet all the requirements of supporting the person with consumer directed care,
- and while you can see that what you are doing is effectively meeting the needs of the consumer, without the accompanying documentation that captures all that has been done, you may be seen as ineffective and non-compliant.
EVV MANUAL CORRECTION (TIMESHEET)
Backup Documentation: If the electronic system is not working, or in the event of manual corrections or edits needed due to missing or incorrect data elements, employee will manually record the following information on timesheet and submit it to the agency:
- Type of service
 provided,
provided, - Name of the Individual receiving the service,
- Date and Location of service delivery,
- Name of the Individual providing the service, and
- Time the service begins and ends.
Recognizing and reporting abuse or neglect
All consumers have the right to be free from abuse, neglect, and exploitation in all settings. These are the fundamental laws that apply to consumers.
There are incidents related to abuse that are clear-cut. But some incidents are not easily identified or understood. Any form of abuse, neglect, and exploitation must be reported.
What is abuse?
Abuse is one or more of the following acts:
- The infliction of injury, unreasonable confinement, intimidation, or punishment upon a consumer with resulting physical harm, pain, or mental anguish.
- The willful deprivation by direct care workers of goods or services necessary to maintain a consumer’s physical or mental health.
- Sexual harassment, rape, or abuse as defined in the Protection from Abuse Act.
- Exploitation by an act or a course of conduct, including misrepresentation or failure to obtain informed consent, which results in monetary, personal or other benefit, gain or profit for the perpetrator or monetary or personal loss to a consumer.
- Neglect of a consumer resulting in physical harm, pain or mental anguish.
Forms of physical abuse include:
- Treating or handling a consumer roughly during care or while transferring, spitting on or near a consumer, or throwing objects at or near a consumer
- Intentionally over or under medicating a consumer, forcing a consumer to swallow medication, forced feeding or depriving a consumer of food or water
- Confining a person (Example, using physical restraints, isolating a consumer
- Denying a consumer access to phone calls or mail, controlling or limiting activities or restricting access to family or friends
Forms of emotional abuse include: 
- Yelling
- Making threats
- Humiliating or ridiculing a consumer
Non-verbal emotional abuse:
- Motioning a threat
- Ignoring a consumer
- Looking at a consumer in a menacing or threatening way.
It is important to remember that body language is a form of communication. So, you must be careful with how you communicate. Even a consumer with cognitive needs, such as a consumer with Alzheimer’s can read your body language.
Forms of Sexual abuse include:
- Rape
- Sodomy, which is anal intercourse
- Unwanted kissing
- Coerced nudity
- Unwanted touching under or on top of clothing
- Penetration of the vagina or rectum with a finder or an object
- Forced oral sex
Sexual harassment is when someone makes unwanted or sexual comments.
Forms of sexual harassment include:
- Verbal harassment
- Sexual gestures
- Direct or indirect comments about a consumer’s genitalia
- Exhibitionism (the act of getting sexual gratification from showing one’s genitals or private areas to others)
- Forcing a consumer to view pornography
- Threatening a consumer if they do not submit to sexual advances
- Taking explicit photos of a consumer
Neglect:
Neglect is a willful defamation by a personal  caregiver or staff of goods or services necessary to maintain a consumer’s physical or mental health.
caregiver or staff of goods or services necessary to maintain a consumer’s physical or mental health.
Forms of neglect include:
- Ignoring a consumer’s care needs
- Not following a consumer’s care plan
- Not reporting new care needs is neglect
Abandonment is another form of neglect.
Forms of abandonment include:
- Desertion
- Purposely leaving a consumer that has care needs unattended
- Conducting personal business outside of the home and not performing the required consumer care and supervision
Exploitation:
- Use of a consumer’s resources without their authorization
- Unexplained withdrawals or other changes to bank accounts
- Disappearance of valuables
- Unauthorized use of a consumer’s property, money, or other items
- Transfer of real estate that does not benefit the consumer
Reporting Requirements:
Agency or employees who have reasonable cause to suspect that a consumer is a victim of abuse shall immediately make an oral report to the area agency on aging (AAA) or the abuse hotline @ 1-800-490-8505.
Within 48 hours of making the oral report, a written report must be completed and sent to the area agency on aging or, if the consumer is under 60, to the designated adult protective services agency.
Employees making oral or written reports must immediately notify the agency manager or designee about these reports. Employees required to report abuse may request the agency or their designees to make or assist in making oral or written reports.
(Source: Temple of University)
Dealing with Difficult Behaviors
As a caregiver, you should know about the consumer and their family by doing a little search before entering the front doors. Seeking help from family members can be very useful in understanding the consumer’s situation better.
Behavioral problems can surface due to many things, such as depression, dementia, and medications. It is vital to handle each situation as appropriately as possible.
Behavioral Problem Criteria:
- Creates danger for the consumer.
- Creates danger for caregivers or others.
- Interferes with essential care.
- Is associated with emotional distress.
Some behaviors that you may find annoying, or offensive should often be tolerated. You will need to find a way to work around the behaviors rather than trying to change them. Here are some tips on what to do under certain circumstances:
Physical Aggression
Physical aggression ranges from pushing you away when trying to provide care to actual assault. No matter what the consumer does to you, you can never retaliate. Back away and use your skills to help the consumer refocus or redirect and calm the consumer down. For example, If the consumer is combative during bath time, a way to redirect would be to try to make it a more pleasant situation. You can explain by saying, “By getting a bath, you will feel much better, and it will give you energy.” If you try to become pushy and insist on taking a bath, this will likely agitate the consumer more. It is very stressful to be a caregiver, especially when the consumer is more combative and aggressive. But you must always deal with professionalism. In this kind of job and situation, panic always happens. You need to pause and step away. Never retaliate. You must consider that if they knew what they were doing, they would not do it. To avoid the situation of confrontation, what you have to do is to join their reality. For instance, if a consumer says I am going to meet my mother today, who died long before and if you say, no, your mother is dead, they will have an adverse reaction and will not believe you.
Another strategy besides making the situation as pleasant and gentle as possible is tapping into the consumers’ natural behavioral patterns. For example, if someone with dementia refuses to shower or bathe, talk to the family about the consumer’s behavioral patterns before dementia. If the consumer would always shower before dinner, set the dinner time for later. The shower now is part of the previous pattern of behavior. This sometimes works better than telling your consumers that they must shower now.
Simple rules to follow to approach any  consumers who might get aggressive safely.
consumers who might get aggressive safely.
- Always approach the consumer slowly from a 45-degree angle.
- Never approach any consumer from behind.
- Smile and make eye contact.
- Identify yourself as a caregiver and explain what you are going to do, always using a calm, soothing, and friendly voice.
- Try not to lean over their body while providing care. That’s when unpredictable incidents can happen, and a caregiver can get hurt.
- Bodily language is also a form of communication. People go with those with whom they feel comfortable. People can get very anxious if your body language is anxious, even though you might be saying all the right words.
- Try not to be impatient and rush.
- Accept who they are. Be flexible with care.
- Always be respectful.
Look For Patterns to The Angry Behavior. Maybe the outbursts always come in the late afternoon when the consumer is more irritable or when you’re in a hurry or stressed.
Try To Break the Pattern. If you can avoid the triggers that lead up to an angry outburst, you can reduce frustration for both of you.
Mealtime: Consumers can become agitated or frustrated at mealtime. Give them a chance to make their own decisions and be in control. For instance, you can ask them:
- “What should we have for breakfast today, oatmeal or eggs?”
- “Do you like your bath before breakfast or after?”
To know if the consumer is eating enough is to watch their weight. If the weight is stable, they are probably eating enough.
Verbal Abuse
- This is not a bad person.
- These are not willful behaviors to make themselves annoying or dangerous to you.
- These people perceive something in their world that you are not seeing or feeling, and that’s why they are acting this way.
- You have to keep in mind that this is not personal. It is not you against them. You have to figure out the best way to provide essential jobs to the consumer. For example, if a consumer says you are fat, it is best not to retaliate. Here is how you could handle the situation instead. Yes, I am fat. Please suggest to me how I could reduce my weight.
Difficult Behaviors
Sometimes you may be in difficult situations. Your consumer may mistake you for his or her partner and approach you in a sexual manner. You have to be professional at all times and address the issue. Do not use aggressive behavior, which may potentially lead to harmful results.
Frustration:
Sometimes, a simple task can be difficult for consumers causing confusion and frustration, leading to aggressive behaviors. Assist them without solely intervening in their ability to do the task they want to do for themselves. Spending quality time with consumers with what they were familiar with, particularly those with dementia, makes a big difference. Treating the consumer with kindness and dignity is important in your role as a caregiver. Treating them as if they are your family members can make a remarkable difference in their behavior toward you. You should be able to feel their time is your time and act accordingly. As a caregiver, you should not take it as your job but instead as two human beings working together. The more you build rapport with your consumer, the more you will be able to serve them in a better way.
Bathing, Shaving, Grooming, and Dressing
Bathing
Helping someone with Alzheimer’s disease take a bath or shower can be one of the hardest things you do. Because these are private activities, people may not want help. They may feel embarrassed about being naked in front of caregivers. They also may feel angry about not being able to care for themselves. Planning can help make bath time better for both of you. If the person is afraid of bathing, follow his or her lifelong bathing habits, such as doing a bath or shower in the morning or before going to bed.
Safety Tips
To keep the person with Alzheimer’s safe during bath time:
- Never leave a confused or frail person alone in the tub or shower.
- Always check the water temperature before he or she gets in the tub or shower.
- Use a hand-held showerhead.
- Use a rubber bathmat and safety bars in the tub.
- Use a sturdy shower chair to support a person who is unsteady to prevent falls. You can buy shower chairs at drug stores and medical supply stores.
Before Bathing
Before starting a bath or shower:
- Get the soap, washcloth, towels, and shampoo ready.
- Make sure the bathroom is warm and well-lighted.
- Play soft music if it helps to relax the person.
- Be matter-of-fact about bathing. Say, “It’s time for a bath now.” Don’t argue about the need for a bath or shower.
- Be gentle and respectful. Tell the person what you are going to do, step by step.
- Make sure the water temperature is comfortable.
- Don’t use bath oil. It can make the tub slippery and may cause urinary tract infections.
During a Bath or Shower
Allow the person with Alzheimer’s to do as much as possible. This protects his or her dignity and helps the person feel more in control. Here are other tips:
- Put a towel over the person’s shoulders or lap. This helps him or her feel less exposed. Then use a sponge or washcloth to clean under the towel.
- Distract the person by talking about something else if he or she becomes upset.
- Give the person a washcloth to hold. This makes it less likely that he or she will try to hit you.
After Bathing
Try these suggestions:
- Prevent rashes or infections by patting the person’s skin with a towel. Make sure the person is completely dry. Be sure to dry between folds of skin.
- If the person is incontinent, use a protective ointment, such as petroleum jelly, around the rectum, vagina, or penis.
- If the person has trouble getting in and out of the bathtub, do a sponge bath instead.
Other Bathing Tips
A full bath or shower two or three times a week is enough for most people. Between full baths, a sponge bath to clean the face, hands, feet, underarms, and genitals is all you need to do daily. Also:
- Washing the person’s hair in the sink with a hose attachment may be easier than doing it in the shower or bathtub.
- Get professional help with bathing if it becomes too hard for you to do it by yourself.
Shaving
Shaving can help your loved one feel clean and well-groomed. It also might help raise their self-esteem and connect them to a daily routine.
Shaving isn’t only for men. As women age, it’s common to grow excess hair on the upper lip and chin. They may want to shave these areas or remove the hair with tweezers. It’s also common for women to have less body hair as they get older. So, they may not need to shave their legs or under their arms.
Allow the person to do the shaving if possible. You can help by gathering the supplies and holding the mirror. If you need to do the shaving, ask if the person wants to be shaved in a certain way, such as starting with the neck and working toward the face.
Getting ready
Start by collecting the supplies you need. You will have to decide if you will use a razor or an electric shaver. For most people, an electric shaver may be the best choice.
Electric shavers are less likely to cause nicks and cuts than a razor. This is especially important if the person is taking medicines called blood thinners, which can cause even minor cuts to bleed more than usual. Also, using an electric shaver may be easier if the person has lost weight, because his or her face may have more angles to shave around. If you feel comfortable shaving your loved one with either a razor or an electric shaver, let them choose which they prefer. It helps to have the person sit in a chair or sit up in bed. But you can shave a person who is lying down if you need to. Make sure the room has lots of light so that you both can see well.
Shaving with an electric shaver 
Place the supplies you’ll need in a spot that’s easy for you to reach. You’ll need a mirror, an electric shaver, and a towel to put on the person’s lap or chest to catch hair. If the person uses a shave lotion for an electric shaver, have that nearby as well.
When you’re ready to begin shaving, follow these steps:
- Wash and towel dry the area you’re shaving. Or use an electric-shaver product that’s made to clean the skin.
- Hold the shaver so that the handle sticks straight out from the area you’re shaving (at a 90-degree angle). If possible, ask the person how they hold it and ask about any special techniques.
- Use back and forth strokes. If you’re using a shaver with round heads (rotary shaver), move the razor in circles.
- Apply moisturizer or aftershave if the person wants it.
- Clean the shaver according to the directions on the package.
Shaving with a standard razor
Place the supplies you’ll need in a spot that’s easy for you to reach. You’ll need a mirror, a razor, shaving cream, and a towel to put on the person’s lap or chest to catch hair and shaving cream. You’ll also need a basin of warm water.
If possible, select a heavier razor. It may help you shave more safely. The weight of the razor helps do the work and may keep you from pressing down too much.
When you’re ready to begin shaving, follow these steps:
- Wash the face with warm water to soften the hair.
- Apply the shaving cream.
- Shave with the direction of hair growth. Shaving against it can cause ingrown hairs and can irritate the skin.
- Press the razor firmly, but not too much. Ask the person how it feels.
- Use short strokes, and be careful around the Adam’s apple, mouth, nose, and chin.
- Rinse the blade after every few strokes.
- Use a warm, moist face cloth to remove leftover lather. Then dry the area.
- Apply moisturizer or aftershave if the person wants it.
- Rinse the razor well before storing it.
Dressing
People with Alzheimer’s disease often need more time to dress. It can be hard for them to choose their clothes. They might wear the wrong clothing for the season. They also might wear colors that don’t go together or forget to put on a piece of clothing. Allow the person to dress on his or her own for as long as possible. Other tips for dressing:
- Lay out clothes in the order the person should put them on, such as underwear first, then pants, then a shirt, and then a sweater.
- Hand the person one thing at a time or give step-by-step dressing instructions.
- Put away some clothes in another room to reduce the number of choices. Keep only one or two outfits in the closet or dresser.
- Keep the closet locked if needed.
- Buy three or four sets of the same clothes if the person wants to wear the same clothing every day.
- Buy loose-fitting, comfortable clothing, such as sports bras, cotton socks and underwear, and sweatpants and shorts with elastic waistbands.
- Avoid girdles, control-top pantyhose, knee-high nylons, high heels, and tight socks.
- Use Velcro® tape or large zipper pulls for clothing instead of shoelaces, buttons, or buckles.
- Try slip-on shoes that won’t slide off or shoes with Velcro® straps.
Grooming
When consumers feel good about how they look, they often feel better. Helping consumers with Alzheimer’s disease brush their teeth, shave, put on makeup, and get dressed can help them feel more like themselves.
Mouth Care
Here are some tips to help a consumer with Alzheimer’s care for his or her teeth and mouth.
- Show the consumer how to brush his or her teeth. Go step by step. Remember to let the consumer do as much as possible.
- Help the consumer clean his or her dentures.
- Ask the consumer to rinse his or her mouth with water after each meal and use mouthwash once a day.
- Try a long-handled, angled, or electric toothbrush if you need to brush the consumer’s teeth.
Other Grooming
Here are some other suggestions for grooming:
- Encourage a woman to wear makeup if she has always used it. If needed, help her put on powder and lipstick. Don’t use eye makeup.
- Encourage a man to shave and help him as needed. Use an electric razor for safety.
- Take the person to the barber or beauty shop. Some barbers or hairstylists may come to your home.
- Keep the consumer’s nails clean and trimmed.
Source: NIH (National Institute on Aging)
Hair: (Source: Family Matters In-Home Care)
Hair care is an important part of an individual’s dignity and self-esteem. Keeping it clean and well-groomed makes a difference in how a senior feel. Seniors may find it difficult to travel to a hair salon, or they may be bedbound. These factors make it important for caregivers to know how to care for a senior’s hair.
The condition of hair in seniors
Aging, stress, and hormonal changes can significantly change the condition of hair in seniors and cause it to grow much more slowly. Hair shedding may increase as the body ages, and the scalp may become dry and itchy. The hair isn’t as elastic as it used to be, and if the hair has repeatedly been processed with perms, coloring, or straightening, it may be dry, brittle, and break easily. With age, the oil glands in the scalp begin to shrink, and that can also contribute to dry hair that falls out more easily.
The best products for senior hair care
Selecting the right products for hair care in seniors can reduce hair breakage and, in some cases, the amount of hair that sheds. Here are the best types of products for senior hair:
- Shampoos with natural oils like argan and/or coconut moisturize the hair.
- Conditioners that have hydrolyzed keratin (protein), and/or olive oil, and shea butter.
- Oil hair masks can add moisture to the hair.
- A boar bristle brush is easier on the hair and may reduce breakage.
Paying attention to nutrition will also keep the hair as healthy as possible. A diet rich in fresh fruits and vegetables high in iron, like spinach, broccoli, lentils, and dark chocolate, is most beneficial.
Whether or not to go to the salon or barbershop
The decision on whether to take your loved one to the salon or barbershop depends entirely upon the status of his or her physical and mental health. If your loved one is mobile and can walk up and down stairs, the socialization of going to the hair salon/barbershop will be beneficial. However, if it is difficult for your loved one to go up and down stairs safely or to keep their balance while walking, it may be time to introduce hair care at home.
Early onset dementia can make it difficult for people to process new environments and multiple conversations. They may forget the person who has cut their hair for years, and they may find the salon/barbershop environment chaotic and difficult to process. If your loved one suffers from any type of dementia, it is important to consider these things when deciding whether or not to continue trips to the salon.
Caring for hair for seniors who are bedbound.
If your loved one is bedbound, washing his or her hair is still possible. Several products can make it easier:
- No-rinse shampoos are easy to use.
- Nurses recommend Sage shampoo caps available on com.
- Nurses also recommend using a specially made hair wash basin. It’s more expensive than the shampoo caps, but something to consider.
How do you wash a bed-bound person’s hair? Here is the technique that nurses use:
- Fold a pillow in half and place it under the top of the person’s back, so it lifts the head enough to place a basin under it.
- Place towels under the basin and on the person’s shoulders.
- Dilute the shampoo in water to make rinsing easier.
- Pour the diluted shampoo on the hair and gently rub it through the hair.
- Rinse it.
- Comb out the hair and dry it gently with a towel.
- Place a dry towel over the pillow until the hair air dry, or use a blow dryer on low, cool air if the person can tolerate it.
- Once the hair is dry, comb it again. For women, you can style it a bit in the front to make them feel good about how it looks.
If you are responsible for caring for your loved one’s hair, it can help to make it a bit of an occasion. Prepare tea, coffee, or your loved one’s favorite drink and a plate of cookies or a healthy snack. Laugh and talk and make hair washing the social occasion it used to be when your loved one went to the salon/barbershop regularly.
Regardless of a person’s age, personal grooming is important part of self-esteem. Looking good leads to feeling good, and that is one reason why hair care for seniors is important and why it can help to avoid depression and isolation.
Skin: (Source: Caregiver Cloud)
One of the caregiver’s most important responsibilities is keeping the consumer’s skin intact and healthy. For consumers who are ill or elderly, proper skin care is essential to prevent serious complications.
The skin is the largest organ of the human body. Let’s look at what it does:
1. It is the physical barrier that protects the rest of the body.
2. It is normally dry, salty, and acidic, which keeps bacteria from growing.
3. It is flexible, moving with the body. Oil glands help keep it lubricated.
As long as the skin is intact and moisturized, it prevents micro-organisms from entering, as well as protects against toxins and chemicals that might be absorbed.
As people age, the skin becomes thin and dry. Small cracks and tears can easily occur, allowing bacteria and other contaminants to invade. Lack of mobility can also cause the skin to break down, leading to pressure sores. Every caregiver must be diligent in helping to maintain skin integrity. Start by keeping your nails short and trimmed, to avoid accidental scratches. Don’t wear jewelry, rings, or watches that might injure the consumer’s skin.
Each encounter with the consumer is an opportunity to evaluate the skin’s condition:
• Baths are the best time to observe the skin. Check for areas of redness, blisters, small cuts, or dry patches. Be sure to note and report anything new or unusual.
• If the consumer is incontinent, excellent perineal care must be given with each episode. The entire area is cleaned, front to back, including all skin folds and the inside of the thighs. Dry the skin well before applying any barrier creams.
• Consumers who have difficulty moving, are bed-bound, or spend long periods in a wheelchair, should be repositioned at least every two hours. During the position change, check the lower back, tailbone, and buttocks for red areas. If present, reposition and check the area in 15 minutes. If it has not disappeared, notify the supervisor or provider. Never massage a reddened area.
• Always keep skin dry by using disposable bed pads. If the consumer uses disposable underwear, monitor for leakage or incontinence. Consumers who perspire will need clothing changes.
• Watch for signs of scratching, which can indicate dry skin. More common in the winter than summer, dry skin often occurs on the hands, arms, shins, and abdomen.
• After bathing or cleaning, dry the skin before applying moisturizer. Adjust the moisturizer to the weather: heavier creams in winter, lighter lotions in summer. Do not apply lotion between the toes; it can promote fungal growth.
• Nutrition and hydration are important for healthy skin. A balanced diet, including high-quality protein, is required to repair and maintain skin. Many ill or elderly consumers do not experience thirst, so encourage fluid intake throughout the day.
As you become familiar with your consumer, checking skin condition becomes a natural part of the day. You’ll notice changes and be able to act quickly to prevent unnecessary infections or discomfort.
Dental and Oral Care: (Source: My Learning Center)
Good oral health and proper denture care play  significant roles in ensuring good overall health in the elderly. Proper dental care has been linked with low incidents of pneumonia in the elderly. Many studies have shown correlations between poor oral health and increased risk for diabetes, cardiovascular disease, and oral cancer.
significant roles in ensuring good overall health in the elderly. Proper dental care has been linked with low incidents of pneumonia in the elderly. Many studies have shown correlations between poor oral health and increased risk for diabetes, cardiovascular disease, and oral cancer.
It is important, as a caregiver, you monitor the consumer’s oral hygiene. Proper care is essential whether they have their teeth, dentures, or implants. Depending on their difficulties may need to assist them with brushing or flossing. Remember that many of the elderly are sensitive to having their mouth, hand, or head touched. Before administering brushing techniques to your clients, explain first what you are doing.
Denture Care:
- Remove their dentures at bedtime.
- Handle dentures carefully.
- Clean dentures regularly. Vigorous brushing, hard toothbrush bristles, abrasive cleaners, and toothpaste can all damage the enamel surface of dentures.
- Keep dentures wet. Keep them in a denture case at night in warm water or a cleaning solution.
- Remind them to care for the rest of the mouth after removing the dentures. Clean the tongue, palate, gums, and the inside of the teeth using fingers or a tooth cleaner. Massage the gums for a couple of minutes to stimulate blood circulation and promote good gum health. Brush the gums in the morning before using the dentures.
- Develop good eating and chewing habits. They should use both sides of the mouth while eating or chewing to avoid wearing out one side of the dentures.
- Encourage them to avoid food that could stain dentures.
If you notice any of the following symptoms, let the consumer’s dentist know.
Warning Signs:
- Bleeding gums
- A change in how their teeth fit together.
- Red, Swollen or tender gums.
- Pus at the gum line of a tooth.
- A change in the fit of dentures or partials.
- Very bad breath.
- A loss of taste or weight loss.
- Loose or chipped teeth.
Dry Mouth:
A dry mouth can also be a problem. As we grow older, several factors are involved in someone’s developing dry mouth. The first is a natural reduction in salvia flow as we grow older. The second is the side effects of many medications as we take more medications.
To keep mouth and lips moist, encourage your client to do the following things:
- Stay hydrated. Helping them to take regular sips of water or other cold, unsweetened drinks.
- Sucking on ice cubes or ice chips.
- Avoid sucking on acidic or sugary foods as they can cause tooth decay.
- Asking the doctor or pharmacist about saliva substitute sprays and gels.
- Sugarless hard candies and chewing gum are two easy solutions that can help minimize dry mouth.
Assistance with Ambulation and Transferring
Ambulation means “walking,” and your client might need to ambulate to get to places or may need to do it to prevent atrophy, which is when muscles waste away from prolonged bed rest.
Other health problems from long-term immobility include decreased cardiovascular and pulmonary functions, poor digestion, pressure injuries, contractures, urinary problems, and many others. So, even if they require assistance, clients are encouraged to ambulate frequently.
Before we talk about ambulation assistance, here are some general considerations.
- Check the client’s chart for information on their most recent ambulation. This will let you know if the client tolerated the activity if they had any difficulty, if an assistive device like a walker or cane was needed, or if they have a history of falls.
- Explain to the client how far you’ll be walking and how you will assist them.
- If an ambulatory device is needed, check to see if it’s functional.
- Make sure the route is not slippery, and there are no obstacles.
- Make sure IV linesand poles are free from tangles and that the IV pump is unplugged from the wall and has enough battery to last during ambulation.
- Make sure they’re properly dressed and wearing non-skid footwear.
- During ambulation, encourage them to walk normally without shuffling or sliding. You might need an additional assistant if the person’s unbalanced, weak, or not cooperative.
- Finally, and most importantly, be sure not to leave the client’s side at any time during the process.
Before getting a resting person to stand and walk, you need to get them into a sitting, or “dangling,” position, where they sit erect with their feet dangling off the side of the bed. The main reason for this is to protect against falling. One common cause of falls is orthostatic hypotension, where blood rushes into the legs as the person shifts into an upright position, causing a drop in blood pressure and decreased blood flow to the brain. It can result in dizziness or even fainting, especially in the elderly.
Transferring
Definition/ Introduction (Source: National Library of Medicine)
Consumer care transfer can be defined as moving a consumer from one flat surface to another. The most common consumer transfers are from a bed to a stretcher and from a bed to a wheelchair. While seemingly intuitive, successful consumer transfers rely on understanding each consumer’s specific needs while simultaneously adhering to evidence-based guidelines. Consumer care transfer can also be defined as transferring consumers within the same facility and between facilities.
Consumer care transfers are an essential yet often neglected aspect of consumer care. Consumer care transfers are an indispensable aspect of consumer care, requiring rigorous adherence to clinical guidelines.
Proper transfers are based on the concept that focuses on maintaining continuity of care both during and after the transfer.
Depending on the complexity, consumers often receive care in multiple settings during and after hospitalization. While some aspects of consumer transport vary depending on the consumer’s status, intrahospital transports are inevitable, particularly in critically ill consumers. Poorly organized consumer transfers can result in increased morbidity and mortality and should be performed with careful attention.
Special considerations:
- Providers should avoid using their weight to lift consumers. Instead, consumers should use their strength during transfers when possible.
- Providers should stay close to consumers at all times during the transfer to keep the consumer’s weight close to the provider’s center of gravity.
- Be careful not to let consumers wrap their arms around the provider’s head.
- If there is a communication barrier, the best resource is demonstrating the transfer using another person. Afterward, the consumer is given hand signals to start the transfer.
Transfer from a Bed to a Wheelchair
Transferring consumers from a bed to a wheelchair requires understanding the needs of the consumer. Always communicate with the person being transferred so that assistance is being given at the appropriate time, allowing for coordination of efforts between the assistant and the consumer. If the consumer can bear weight on both lower extremities and predictably take small steps, a one-person assist may be performed. If these criteria are not met, a two-person transfer or a mechanical lift may be necessary to safely transfer the consumer. If transferring a consumer from a bed to a wheelchair, first complete the pre-transfer checklist and proceed according to the following steps:
- Apply the consumer’s footwear before ambulation.
- Raise/lower the bed to a safe working height, lower guard rails, place wheelchair next to the bed at a 45-degree angle and ensure the brakes are applied. If one side of the consumer is weaker, place the wheelchair on the healthier side.
- Sit consumer on the side of the bed with the legs off of the bed and the feet squarely on the floor. If necessary, attach a gait belt/walking belt around the consumer’s waist.
- Place hands on the consumer’s waist.
- The provider positions his/her legs on the outsides of the consumer’s legs. As the consumer leans forward, bending at the waist, the provider grasps the gait belt (or the consumer’s waist).
- Help the consumer shift weight in a rocking motion (front foot to back foot, and so on) until reaching a standing position.
- Once the consumer is standing, have them walk a few small steps backward until feeling the wheelchair’s back against the legs. Ask the consumer to grasp the wheelchair.
- The provider will shift their weight from back to front as the consumer sits in the wheelchair slowly, using the wheelchair’s arms for support.
- Ensure that the consumer is adequately draped and sitting comfortably in the wheelchair.
- Consumers may use slide boards for more effortless transfer.
- When the consumer transfers back to the bed from the wheelchair, the safest sequence of actions is positioning the chair at a 45-degree angle to the bed, locking the brakes, raising the footplates, and rotating the leg rests outward. Only after the correct sequence is performed can the consumers scoot to the front of the wheelchair. When the consumer scoots forward, the body is positioned over the feet. This will allow the consumer to stand more easily. Leaning forward or grasping the edge of the bed is likely to cause the wheelchair to tip forward. Assistance can be given to block the person’s knees to provide additional support.
Ambulation: (Source: OSMOSIS from ELSEVIER.
Contributors: Zachary Kevorkian, MSMI, Ph.D., Evan Debevec-McKenney)
Meal Preparation and Feeding
Meal Preparation
Practice good food safety.
- Wash hands well before handling food.
- Cook food thoroughly and cook meats to the proper temperature.
- Do not reuse utensils or surfaces that have come in contact with raw meat.
Small may be better.
- Consumer may not have much of an appetite, so smaller portion sizes may be the way to go.
- Serving small meals frequently through the day allows for better digestion, fewer stomach upsets, and more energy.
- Use smaller plates and cups to help control portion size.
Ask for requests.
- If you are preparing a meal as a caregiver, check with consumer to see what food and drink sound good.
- Try to avoid serving the same thing every day unless the consumer requests it.
Avoid fat.
- Prepare food by baking, slow-cooking, grilling, or broiling to limit fat. Fats can make some digestive issues worse.
- But there is an exception! If the consumer needs to gain weight or stop losing weight, add healthy fats and oils to add extra calories to the food.
Check the spices.
- Changes in taste and smell are common side effects of cancer treatment.
- Check in with the consumer. You may need to adjust or change spices for changing tastes.
- If consumer complains of a metallic taste, switch to plastic utensils and plates.
Keep aromas to a minimum.
- Sensitivity to smells or odors is another side effect of cancer treatment. If the odor is an issue, cook while the survivor is out of the house or asleep.
- Use fans to move food aromas, and cooking smells out of the kitchen and house.
- A small personal fan at the dinner table also may be helpful.
- Prepare cold meals like sandwiches, fruit and cheese plates, crackers with peanut butter and celery, and smoothies.
- Use cups with lids and straws.
- Use a Meal Planning Worksheetto plan meals in advance.
- Friends and family may want to help prepare meals. Keep a list on the refrigerator of who is bringing what and when.
- Label prepared foods with an eat-by date.
- You can also use online resources to help with meal planning and coordination.
Feeding
Someone who cares for the elderly on a respite or ongoing basis is called a caregiver. While caregiving can be rewarding for a compassionate person, the demanding job of properly caring for and feeding the elderly can also be draining. To lessen the physical and emotional demands of the job, caregivers can structure their day with a schedule, detailed notes and necessary breaks. Consumer well-being is enhanced through careful attention to their social, emotional, and physical needs.
Sip liquids between meals.
Staying hydrated is important, so let consumer one sip liquids between meals, but stop drinking 30 minutes before a meal or snack to build an appetite.
Drinking too much at a meal, especially low-calorie beverages, can replace vital nutrient dense foods like meat, vegetables, and fruits.
Limit drinks with meals so more solid foods with calories can be consumed.
Serve moist foods.
Foods with moisture, like tomatoes, fruits, other vegetables, gelatin, soups, puddings, and ice cream, all provide water. So, the consumer won’t need a big glass of water with the meal.
Moist foods require less cutting and chewing, which conserves energy to eat the rest of the prepared food.
Moist foods are also easier to swallow.
Use pictures of food to stimulate appetites if the consumer doesn’t want to eat.
Seeing food advertisements and magazine pictures can help stimulate the appetite or trigger memories of good meals.
Share your magazines or grocery store ads with the consumer and use them for meal ideas.
Be social.
Meals are only healthy and nutritious if the consumer consumes them. Making meals social and fun can help with appetite.
Following a Predictable Schedule
Repeating the same daily tasks at the same time gets the caregiver and consumer on the same schedule. This is beneficial because both parties know what to expect, which in turn reduces complaining and power struggles. In addition, a schedule means efficient use of time; medication is given when necessary and the caregiver is better able to manage unexpected issues.
Responding Compassionately to Needs
It’s natural for someone needing care to still desire certain foods or things that a doctor has warned against. For this reason, a caregiver needs to pay particular attention to certain activities or foods that the consumer could still engage in but are not safe or healthy. Understanding a consumer’s health condition helps maintain the relationship with the consumer while protecting consumer health.
For example, consumers on dialysis may experience extreme thirst even though liquids must be limited for kidneys to work efficiently. A caregiver can respond to this situation by pointing out that the glass of water is too full and suggesting that the consumer suck on an ice cube instead of drinking water.
Encouraging and Praising Independence
While a caregiver is there to assist the consumer, it’s also important to encourage independence. It is not a caregiver’s job to strip consumers of their dignity or their decision making. rather, you’re there to support what they can do and encourage their autonomy and independence as far as possible.
In addition, it’s a good idea to take notes so that you can give gentle reminders to the consumer, such as the importance of exercising or asking if she would like to rinse her mouth after eating. This encourages healthy behavior, without limiting the consumer’s decision-making abilities. Praise effort and progress.
Properly Feeding the Elderly

A consumer’s dietary needs must be taken into consideration, such as a low-salt diet or foods to avoid because of religious reasons. In addition, careful attention should be paid to the consistency, temperature and texture to keep dental work in place and prevent choking. Proper feeding techniques include cutting up foods in appropriate sizes. Best foods for dementia consumers to eat are finger foods and small bite size portions, according to dementia specialists.
The U.S. Department of Health and Human Services Foodsafety.gov website cautions that older adults are at increased risk for life-threatening food-borne illnesses due to aging bodily systems and underlying health conditions. Aim for a variety of properly prepared, enjoyable and nutritious foods that are presented in an attractive way. Loss of appetite in elderly consumers can lead to weight loss, poor nutrition and a weakened immunity system.
Giving Proper Care and Attention
Caregivers need to be consumer when helping the elderly eat, bathe, dress, use the restroom and do any kind of activity. When eating, for example, position the person with her head slightly flexed and the chin downward, and adjust her seat to the right table height. Those with visual impairments should be guided gently when stepping into a shower and wiping the mouth, for example.
In addition, giving emotional attention is crucial to the caregiver-consumer relationship. A consumer feels loved and needed when the caregiver respects her opinions and understands her situation.
Meal Preparation
Source: (https://pearlpoint.org/food-prep-tips-for-caregivers)
Feeding
(Source: work.chron.com/caregiver-feeding-tips-elderly-15030.html)
Toileting
Seniors may need help getting on and off the toilet
Even if your older adult is pretty independent, they may still need a little help when they go to the bathroom. It’s easy for seniors to fall when walking to the bathroom in a rush or when sitting or standing [on or] from the toilet due to blood pressure changes.
Basic safety tips for elderly toilet use
- Encourage them to move on their own as much as possible to reduce the chance of injury for both of you. You’re mostly there for balance support.
- Never lift your senior outright or ask them to pull on you. This is likely to cause injury to one or both of you.
- Hold on to their trunk and hips to keep them stable. Don’t pull their arms or legs, that could injure fragile extremities or throw them off-balance.
- Always bend your knees when supporting them as they lower or raise themselves. If you bend at the waist, you risk injuring your back.
Clear communication is essential
Before moving, use short sentences to explain the next step so your older adult knows what to expect. And give them plenty of time to do what you ask.
Examples:
- The toilet seat is right behind you. Squat down slowly to sit.
- I’m going to help you stand up now. Scoot your butt forward.
- Lean forward and put your hands on my forearms when you’re ready.
Getting to the bathroom safely 
- Allow your older adult to walk at their own pace but stay close and be ready in case they wobble or trip.
- Once they’re near the toilet, ask them to use small steps to slowly turn around until the toilet is directly behind them.
Daily Caring tip: Getting to the bathroom safely can take some time. To reduce the chance of an accident because getting to the toilet takes longer than expected, make regular trips to the bathroom to reduce urgency – try after meals and every couple of hours.
How to sit and stand safely
- Ask them to lower themselves slowly onto the toilet seat while placing their hands on your forearms. Steady them with your hands on their trunk. Bend your knees as they lower themselves.
- Before standing up, ask them to scoot forward a little and place their hands on your forearms before slowly raising themselves up. Keep your hands on their trunk and bend your knees.
- Don’t let them hold on to their walker as they sit or stand because it could tip over and cause a fall.
Source: https://dailycaring.com/safety-tips-elderly-toilet-use
Assistance with Self-administered Medication
A critical responsibility of a Direct Care Worker is ensuring the health and well-being of the consumer. In some cases, this includes ensuring that medications are taken correctly. If you are unsure about assisting a person in taking his/her medication(s), stop, contact your supervisor or other person designated by your agency, and get clarification before you continue.
Who can self-administer medications?
To be considered able to self-administer medications, an individual shall do all of the following:
- (1) Recognize and distinguish the individual’s medication.
- (2) Know how much medication is to be taken.
- (3) Know when the medication is to be taken.
- (4) Take or apply the individual’s own medication with or without the use of assistive technology
Where to find information about providing assistance with medication self-administration?
The consumer’s Individual Care plan (ISP) provides support information about medication(s) taken and the amount of assistance needed for medication self-administration. The ISP states whether the consumer needs assistance in the self-administration of medication and any special instructions about the type of assistance:
- Requires no assistance in the self-administration of medication or medication administration.
- Needs assistance in the self-administration of medication, which can include:
- Reminding a consumer that it is time to take a medication;
- Opening a medication container for a consumer.
- Pouring or placing a specified dosage as instructed by the consumer into the consumer’s hand;
- Observing the consumer while the medication is taken; or
- Assisting the consumer to take the medications that have been prepared in advance in a medication organizer by the responsible person.
- Needs total assistance, which includes the use of medication organizers.
- Medication organizers may be prepared in advance by the responsible person. There need to be clear, simple instructions from the responsible person. Example: The medication needs to be in a container that is clearly marked, “Please give to my mother at 10 am with a glass of water.” (Only the exact dose is in the container so that the DCW does not have to decide how many pills to use.)
Documentation
The Direct Care Worker must keep documentation by recording the date and time of day when assistance with medication self-administration was provided. Document that medications were administered according to the consumer’s instructions or the medication organizer’s date and time, as directed by the responsible person.
What you cannot do:
- A DCW cannot use professional judgment and cannot make decisions about medications.
- If the consumer does not know which medication is which, the DCW cannot help figure this out.
- If the consumer is confused about dosage/time etc., the DCW cannot help sorting it out.
845 Sir Thomas Ct. Suite 9
Harrisburg, PA 17109
Phone: (717) 317 9037
Fax: (717) 798 3144
contact@milestonehomecare.com